Eye Conditions
Topics:
Eye Conditions Overview
Eye Condition Ratings
Eye Conditions Overview
The VA awards disability compensation for eye conditions that are service-connected. The DoD will also rate service-connected eye conditions as long as they also make the service member Unfit for Duty. For Reservists, the eye condition must have occurred in or resulted from an injury in the Line of Duty to qualify.
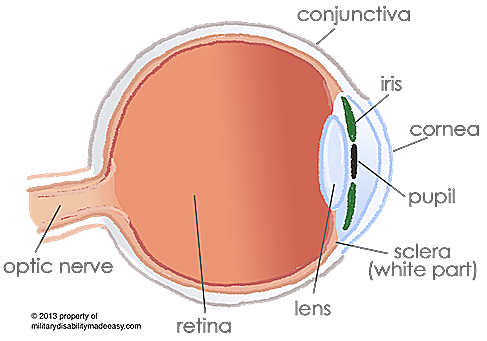
The Eye is a complex sensory organ consisting of many layers that combine together to create a vast network of sensors that enable three-dimensional sight. Our quality of vision is determined by how well our eyes can focus on an image (visual acuity), how well the muscles can control the movement of the eye (muscle function), and the quality and extent of the visual range that can be seen (visual field).
Because of the complexity of the eyes, the VASRD offers rating options that cover physical damage to individual parts of the eyes, options to rate on incapacitating episodes based on the number of treatments needed to treat the condition, and options that cover conditions affecting one, two, or all three areas of visual impairment (visual acuity, visual field, and muscle function).
To honor the Pyramiding Principle, only a single rating can be given for multiple eye conditions since it is basically impossible to separate the symptoms. In situations where multiple conditions are present, the eyes will be rated using all of the symptoms combined together to reflect the overall functioning of the eyes. Any exceptions to this rule will be noted directly in the code to which it applies (see The Eye Ratings page).
Return to Top
Eye Condition Ratings
The VASRD offers ratings for the following conditions of the Eyes:
- Loss of the Eye
- Loss of Vision
- Conditions affecting the Visual Field of the Eyes
- Conditions affecting the Muscle Function of the Eyes
- Diseases of the Eye
- Conjunctiva Conditions
- Corneal Conditions
- Retinal Conditions
- Lens Conditions
- Nerve Conditions
- Eye Conditions Caused by Brain Damage
- Conditions of the Eyelids and Tears
- Loss of the Eyebrows and Eyelashes
- Tuberculosis of the Eye
- Cancer and Tumors of the Eye
If an eye condition is not directly listed, it is rated under the code that best describes it or its dominant symptom.
Blindness in both eyes or in a single eye when combined with other disabilities may also qualify for Special Monthly Compensation.
Return to Top
FAQs
How will the VA rate my eye conditions?
The VA uses the rules of the VASRD to rate eye conditions based on the level of disability remaining after the use of glasses or contacts. Check out our Eye Ratings page for the exact codes and ratings.
My condition wasn't diagnosed until after I was discharged. Can it qualify for VA disability?
The VA can only rate conditions that meet some type of service-connection requirement. For conditions diagnosed after service, the condition must either be a secondary condition caused by another service-connected condition, or it must be on the VA's Presumptive List.
Are my conditions eligible for a rating?
Your conditions are eligible to be rated by the VA if they are the result of your military service. You must be able to show proof of service-connection for each condition. For the DoD, they will rate your service-connected conditions as long as they also make you Unfit for Duty.
How do I apply to receive my ratings for my eye conditions?
If you are still in the military, then you can request your military physician to refer you to the MEB and start the IDES process. If you are already a veteran, you can submit a VA Disability Claim along with evidence of service-connection and all medical records regarding the conditions on the claim.
If my claim is approved, what benefits will I receive?
If you are rated 20% or less from the DoD, then you will receive a single separation payment. If you are rated 30% or more, you will receive full retirement benefits. From the VA, you will receive a monthly payment as well as full medical care from the VA for the qualifying conditions.
How long does it take to receive my disability benefits?
Brand new claims usually take 3-6 months to process. Once processed, you will start receiving payments in 1-3 months.
How are the rating percentages assigned to my conditions?
The rules of the VA's Schedule for Rating Disabilities (VASRD) are used to assign rating percentages to conditions. The VASRD gives rating rules for conditions based on their symptoms, treatment options, and the resulting level of disability they cause.
My conditions have worsened. How do I increase my rating percentages?
If your conditions have worsened since you last applied and now qualify for a higher rating, you can submit a new claim, checking the box for an increased evaluation.

